EYEREUM was chosen as ‘Korean KERARING Center of Excellence’ by the global medical company, Mediphacos Inc., for our continual success in keratoconus treatments. And in 2015, EYEREUM was awarded ‘Master of KERARING in South Korea’ for the most number of Keraring implants.
Also, the chief director, Dr. David Kang(David Sung Yong Kang), was appointed one of the 15 Medical Advisory Board members by the American Avedro Inc., which possesses the cross-linking technology in treating keratoconus. He is currently the ambassador in Asia and has worked together with world renowned medical specialists.
EYEREUM has worked with the world’s best keratoconus experts not only to treat keratoconus but also to establish a global safety standard to prevent any side effects. EYEREUM is taking the lead to provide domestic patients with advanced medical technology.

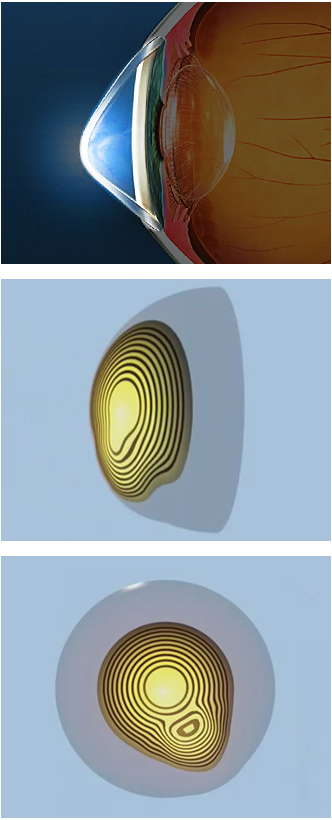
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. The exact cause of keratoconus is not yet known, but it usually starts in the teenage years. It can, though, begin in childhood. Also after vision correcting surgery, the abnormally thin cornea can’t withstand the eye pressure and the area below the center of the cornea starts to bulge. This is the most devastating complication after any laser eye surgery and occurs when the minimal corneal thickness was not preserved.
This is why the American FDA has emphasized the safety standard corneal thickness to be 250㎛. EYEREUM, however, leaves more than 400㎛ when performing laser surgery in case of re-operation and shows this result to our patients. As for symptoms, the center of the cornea starts to bulge slightly downward and the cornea becomes a cone shape. This causes progressive astigmatism to develop, creating additional problems with distorted and blurred vision. As keratoconus progresses, the cornea can rupture making interior become murky, or there could be scarring. Also Fleishcher’s ring, a pigment deposition, at the base of the cone, is present. Usually there aren’t any particular subjective symptoms like pain, however some patients do experience blurred vision or glare. As the disease worsens, keratoleucoma may occur, leading to blindness.
Recently, corneal collagen cross-linking (CXL) procedure is in the limelight, as it, like the corneal ring implants, is known to prevent ectasia.
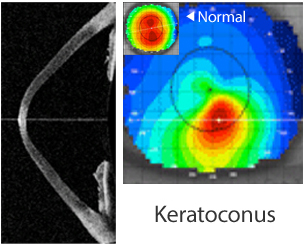
1. Keratoconus
Unlike corneal infiltrate which is inflammatory, keratoconus is non-inflammatory. It is a progressive disease in which the normally round cornea thins and begins to bulge into a cone shape, causing irregular astigmatism.
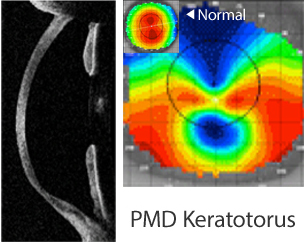
2. PMD Keratotorus : (Pellucid Marginal Degeneration)
PMD Keratotorus, is a degenerative corneal condition, often confused with keratoconus. It usually affects only one eye, and is typically characterized by a clear, bilateral thinning in the inferior and peripheral
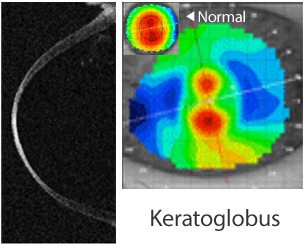
3. Keratoglobus
Keratoglobus is a degenerative non-inflammatory disorder in which the cornea gradually becomes extremely thin and changes to a more globular shape. It is caused primarily due to corneal thinning at the margins.
1. KERARING Surgical Treatment
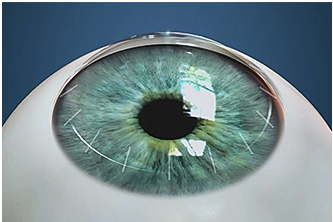
Advanced keratoconus patients may not be able to get adequate vision correction with contact lenses anymore and may need to find other treatment. One of those treatments, before considering corneal transplantation, is an intrastromal corneal ring (KeraRing) implant. This implanted ring flattens the cornea and reduces myopia as well as treats keratoconus. One or two rings are inserted into the cornea to reshape the front surface.
The KeraRing implants have the advantage of being removable and exchangeable. However implants are not recommended for those whose corneas are too thin. Although the implants can also correct astigmatism, as they are inserted much closer to the pupil, there is a possibility of blurred vision. This problem has been amended by designing the cross section to a prism shape. And for this technology, KeraRing has gained the European CE mark and has been KFDA approved.
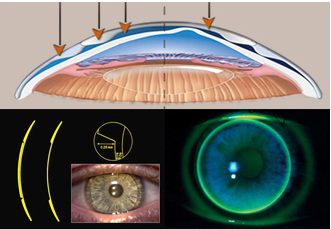
2. Collagen Cross-Linking Surgery
The cornea consists of mostly collagen, which is one type of protein found in our bodies. The collagen cross-links together and is responsible for preventing the cornea from bulging out and retaining its normal shape. In patients with keratoconus, the collagen tissues become weak, causing the cornea to thin and bulge out. Corneal collagen cross-linking (CXL) strengthens corneal tissues to cease the bulging.
During the corneal cross-linking treatment, riboflavin (Vitamin B2) drops saturate the cornea, which is then activated by ultraviolet light to strengthen the collagen cross-linking in the cornea. Collagen cross-linking arrests progression of keratoconus, and thereby prevents further deterioration in vision. The irregularly bulging cornea will then return back allowing the patient to wear contact lenses or glasses. Some patients have said to have even experienced a better vision. This procedure strengthens the cornea and basically and physiologically treats keratoconus. Also it can be used together with corneal ring implantation, such as Intacs or KeraRing to enhance its effects.
3. Cornea Transplantation
More than 25% of keratoconus patients are in a severe stage that they need a cornea transplant. This is the most traditional treatment method which involves removing the center of the cornea and replacing it with a donor cornea. However, if the cornea transplant shows rejection, there could be serious complications. After a cornea transplant, 80~90% of patients gain a stable vision. But some might be left with a degree of astigmatism, which can be corrected with contact lenses or glasses. The new vision will fluctuate during the first few months following the surgery. And it will take more than a year for a completely recovery.
4. Non-surgical Treatment: RGP Contact Lenses
RGP (Rigid Gas Permeable) contact lenses mask the underlying irregular cornea and function as a new refractive surface of the eye. They are custom-made for each patient in order to correct vision. There are other contact lenses for keratoconus; however, if vision cannot be corrected with contact lenses, cornea transplant is the last resort.
-
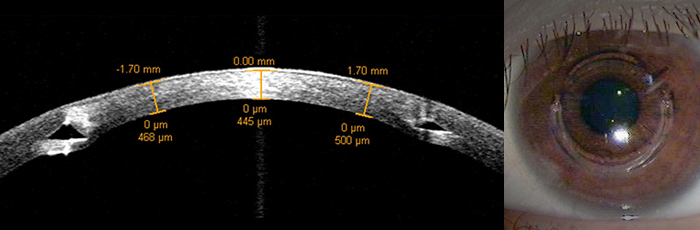
A university student, Kim, with both hyperopia and keratoconus Consulted with EYEREUM not to correct vision but to treat keratoconus
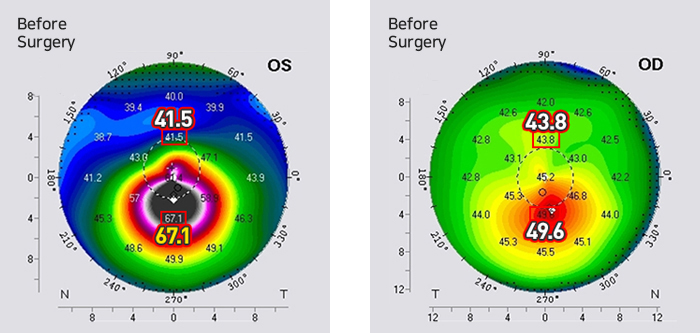
Stage 1 : Corneal Ring Implant, KeraRing
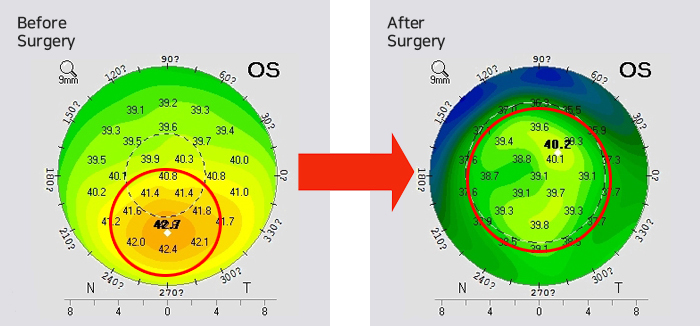
In December 2014, KeraRing surgery was performed on the left eye, which was suffering from serious keratoconus.
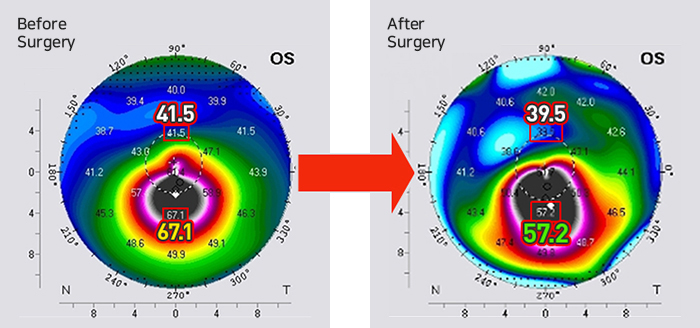
Stage 2 : Cross-linking & CoWave
5 months later cross-linking and ARAMIS RED CoWave were preformed to stabilize the vision. Kim was not only having difficulties but was also scared to do everyday tasks. Kim was mostly afraid of the possibility of going blind. However, after treating keratoconus and correcting hyperopia, Kim is excited to be able to see clearly and live a normal life.
-

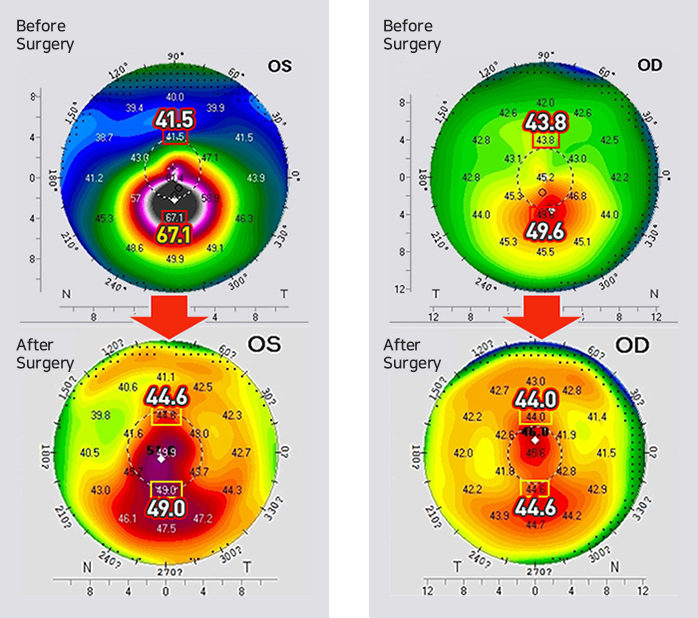
26 year-old Chang, who was diagnosed with keratoconus in Daejeon, came to EYEREUM to treat it.
Stage 1 : Right eye: Corneal ring implant (KeraRing)
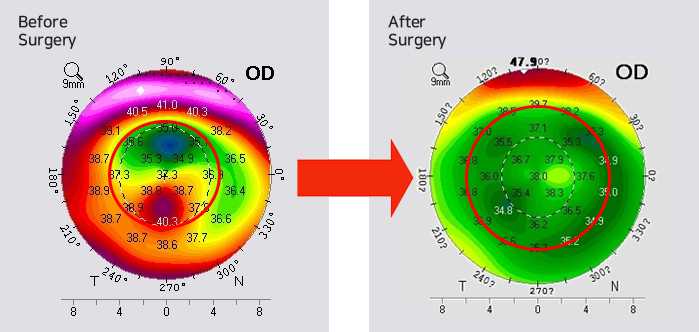
KeraRing surgery was performed on the right eye with severe keratoconus.
Stage 2 : Left eye: Cross-linking & CoWave
Both collagen cross-linking procedure and CoWave surgery were performed on the right eye to correct the asymmetric cornea.
-

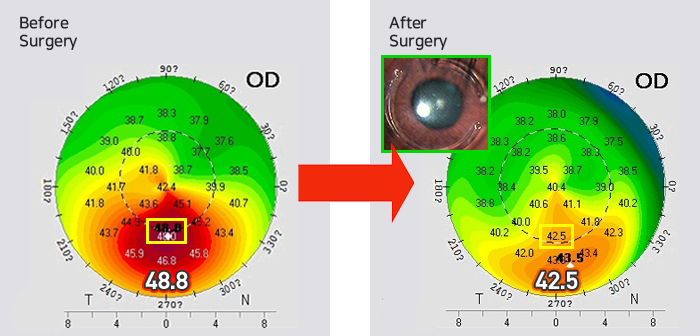
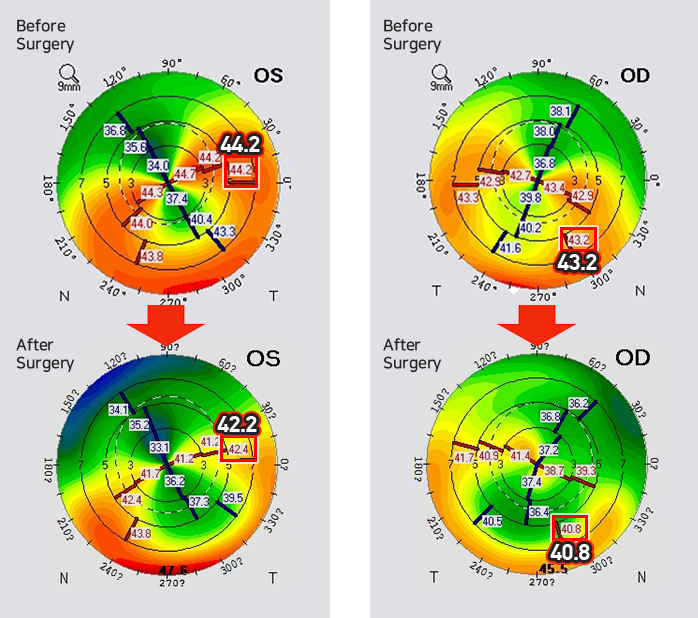
After having LASIK surgery in another clinic, Park visited EYEREUM because of Central Islands in the right eye.
Corneal ring implant - Right eye (KeraRing)
Park had severe Central Island in the right eye with visible corneal opacity and possible corneal enlar-gement. With cross-linking treatment and CoWave surgery, Park’s cornea has been stabilized by sym- metrizing it and the progression of corneal enlargement has been prevented. Park’s vision was stable by August, 2015, and as only one eye was treated, currently the vision in both eyes is crystal clear.
-

Park experienced sudden vision loss within a year and even had undergone several examinations at a university hospital before coming to EYEREUM. After more extensive examinations, Park was diagnosed with progressing PMD keratotorus, which is different from keratoconus.
Both eyes: Cross-linking & CoWave
The development of the progressing PMD was halted with cross-linking.
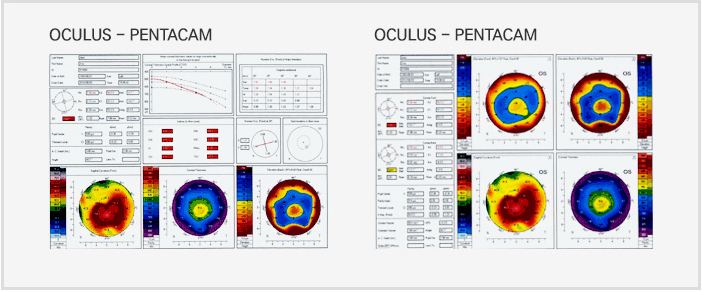
Corneal enlargement can be diagnosed with the following examinations: slit-lamp biomicroscopy, retinoscopy, keratometer, corneal topography etc. The corneal topography examination is especially helpful in diagnosing early keratoconus.