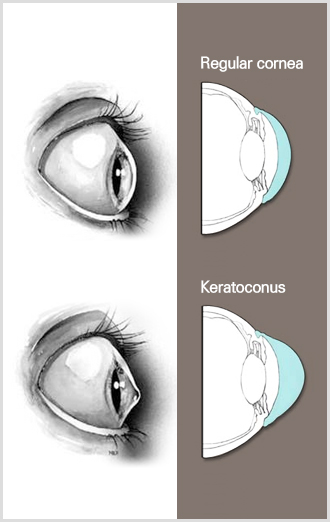
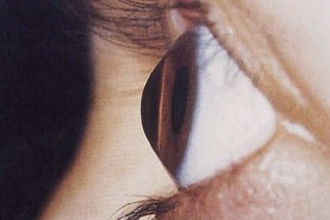
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. The exact cause of keratoconus is not yet known, but it usually starts in the teenage years. It can, though, begin in childhood. As for symptoms, the center of the cornea starts to bulge slightly downward and the cornea becomes cone-shaped. This causes progressive myopia and irregular astigmatism, creating additional problems like distorted and blurred vision. As keratoconus progresses, the cornea can rupture and the interior becomes murky. Also Fleischer’s ring, a pigment deposition, can occur at the corneal conical base. Usually there aren’t any particular subjective symptoms or pain, however some patients do experience blurred vision or glare. If left untreated, keratoconus may lead to blindness.
You may feel your overall vision deteriorating as you experience both myopia and hyperopia . Also, you may start having distorted or blurred vision due to astigmatism and become more sensitive to light. This may lead to poor night vision and severe dry eyes. If there is a large difference in vision and refraction between both eyes, or if you have had to frequently change your eyeglass prescription or have not been able to correct your vision even with glasses, you should consult a specialist and have a comprehensive examination.
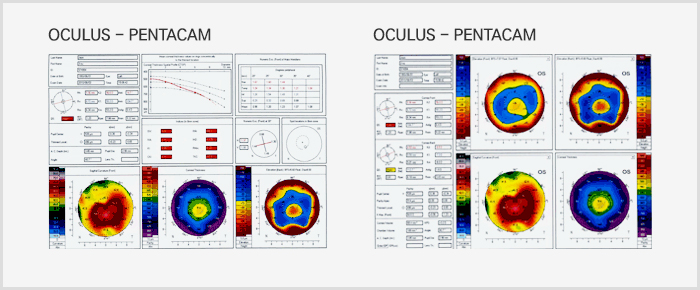
There are several tests for determining keratoconus, including slit-lamp test, retinoscopy, the corneal curvature test, ultrasound biomicroscopy and the corneal topography test. Among these tests, the corneal topography test is the most effective in diagnosing keratoconus in the early stages.
- Non-surgical Treatment: RGP Contact Lens
- Surgical Treatment: Intrastromal corneal ring implantation (KeraRing), Collagen cross-linking, and Corneal transplantation



